Introduction
Last two decades have seen emergence of minimalism in spine surgery to minimize the approach related trauma of the tissue. MISS – “minimally invasive spine surgery” phrase is nowadays quite often used. In fact it is a misleading terminology, because MISS surgeries are potentially maximally invasive at the target area. There is no compromise in achieving the exact goal, that is adequate decompression of compressed neural structures in MISS. But the approach related trauma to surrounding tissue is minimized.
It really does not matter what technique you use to decompress the nerve root, if you fail to fully decompress the nerve root or introduce complications to the equation, you have failed to serve the patient.
- Ian MacNab
One should try to follow this principle in spine surgery. In minimally invasive spine surgery while following this philosophy each and every patient’s symptoms, clinical signs and radiology has to be evaluated separately and carefully. If the decompression of the compressed nerve root / cord is inadequate, then the compressive symptoms, signs will persist. If the decompression is aggressive or more than necessary then there are chances that the existing stability is compromised. Hence there has to be nice equilibrium between adequate decompression without compromising the existing stability. This equilibrium will be different for every patient, every level to be operated, extent of stability / instability & the pathology to be treated. This is dependent on each spine surgeon along with the technique used by the surgeon. This is one of the many factors which is responsible for steep learning curve in MISS – Endoscopic spine surgery.
Destandau’s technique
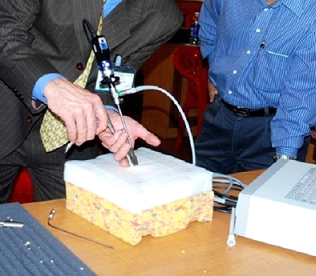
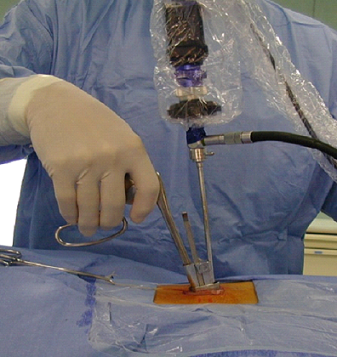
Dr. Jean Destandau M. D. neurosurgeon from Bordeaux France, developed a technique of endoscopic spine surgery in 1993. ( 1, 2). This technique is based on basic principle of laparoscopic technique of triangulation between an endoscope and suction with working instrument.
Basics of Endospine – Destandau’s technique.
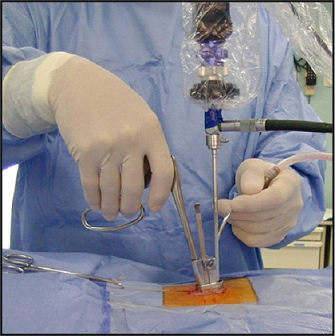
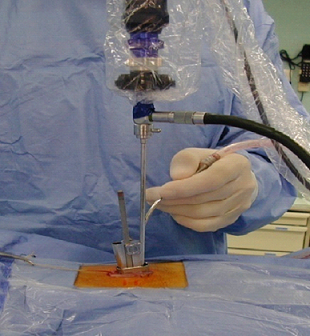
In Destandau’s technique we use Endospine, a set of outer tube / insert and inner tube / working insert with an endoscope. The endoscope used with endospine is 18 cm’s, long, rigid, straight, 0 degree endoscope. One can say an universal endoscope which used in cystoscopy, arthroscopy, sinoscopy etc. The outer tube is elliptical in shape rather than circular. Endospine was initially used for lumbar disc herniation. The target area in lumbar region is elliptical, in between two laminae, medially the spinous process and laterally the medial facet, hence the outer tube might be of elliptical shape rather than round. The inner tube / working insert fits in to the outer tube with a rachet type lock. There is an inherent telescoping movement in between these tubes.
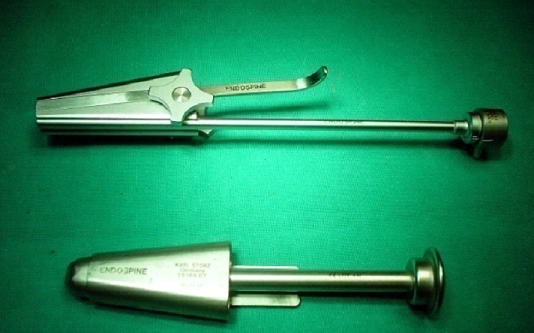
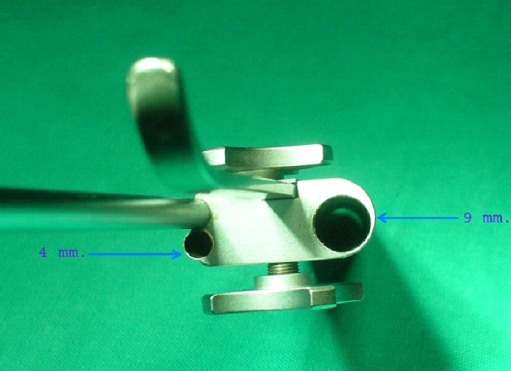
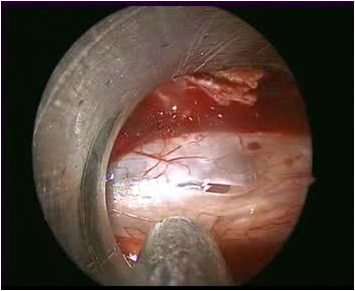
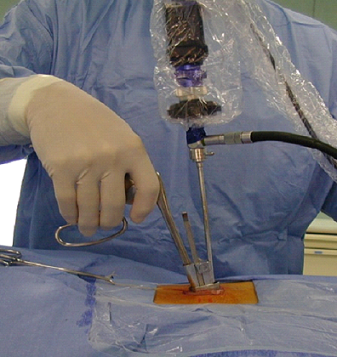
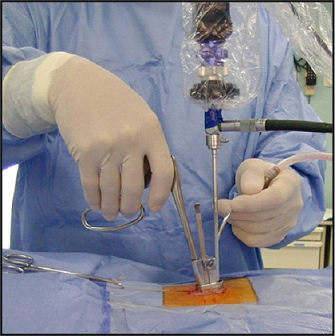
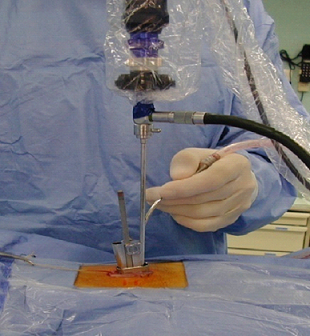
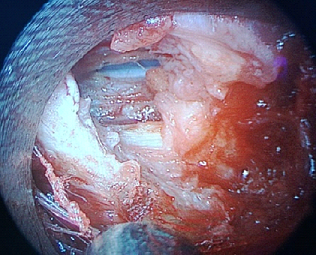
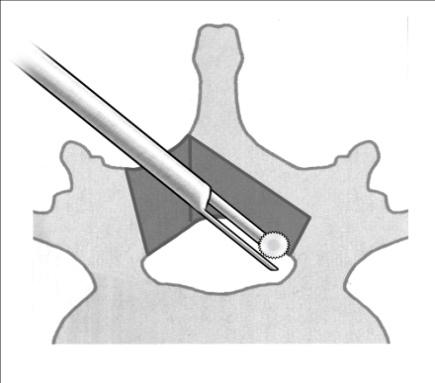
The working insert has four in build channels inside. On the left side of the working insert it has two channels of 4 mm diameter which are parallel to each other. The medial 4 mm channel hosts the endoscope and then the endoscope remains fixed with lock. The second 4 mm channel is for suction tube. The largest channel of 9 mm is for working instrument. The channels for endoscope and suction, is at an angle of 12 degrees to the wide channel for instrument. Because of this angle we can use 0 degree endoscope as an angled scope. This helps in minimizing the fogging of endoscope tip. When the endoscope and the instrument are working parallel to each other there is intermingling of the instruments. And we have to use an angled endoscope when endoscope and instrument work parallel to each other. The fourth channel is for nerve root retractor to retract the nerve root medially so as to expose disc space. The outer tube and inner tube are fixed in such a way that there is an artificial space created in between the two tubes. This is the working space for the instruments. Once the excision of the bone is achieved then the inner tube can be pushed inside/down. If there is no space maintained in between the outer tube and inner tube then the endoscope will touch to the tissue in front and will hamper the vision. Also there will be splashing of fluid over the endoscope lens if adequate space is not maintained in between these tubes. The suction is used with left hand and working instrument is in the right hand. With suction in left hand surgeon can move whole system in medial, lateral, cranial and caudal direction. Same movements are possible with instrument in right hand. The suction in left hand and instrument in right hand work as breaks for the system to maintain the stability of the system. When the surgeon is using suction to clean the operative area, the instrument in right hand keeps the system stable, vice versa when surgeon is using instrument, suction in left hand keeps the system stable. This synchronisation of movements of both hands, is necessary while looking at the image on the screen. Surgeon should learn this synchronisation of both hands movements, along with using of both hands while looking at the screen image. This is the basic’s of the Destandau’s technique is spine surgery. ( 1 ).
Endoscopic Lumbar Discectomy - Destandau’s Technique
Various positions are used in lumbar spine surgery for discectomy, such as prone position, lateral position, and knee-chest position. Prone and knee-chest positions are natural positions for use of Endospine. Lateral position is not natural as it does not support the Endospine system. In between prone and knee-chest position the author preferably uses knee-chest position. Knee-chest position can be used with folding the operating table at 90 degrees. Author, Dr Shrinivas Rohidas uses a different knee-chest position, in which the patient is positioned on a rectangular pillow that supports the head and upper chest so that the head is lower than the caudal end due to the angulation provided by pillow. There is pillow at the knee in between the thigh and calf. Another pillow is underneath the ankles. The abdomen is completely lax in between the thighs with added interspinous distraction. The head is lower than the caudal end, which allows natural venous flow of abdominal epidural veins towards the heart by gravity. The interspinous distraction is useful in cases of spinal canal stenosis. In patients with osteoarthritis of knee and hip in which flexion at the knee and hip is restricted, it is not advisable to adopt this particular knee-chest position used by Dr. S. M. Rohidas. In these patients he uses prone position with the help of bolsters. For Asians it is quite easy to use this modified knee-chest position as they are accustomed to sit on the ground for meals and also for stretching exercises such as padmasana or vajrasana. Also, the Asians use these positions during prayers such as namaj. This particular knee-chest position stretches the laminae. This can be disadvantageous in a patient with huge central disc herniation in which the huge disc has already stretched the dural sac and nerve root. Because of interspinous distraction in knee-chest position, there can be more stretch over already stretched dural sac and nerve roots. Hence during surgery we have to be sure that the concerned nerve root is adequately decompressed so that one can see the axilla and shoulder of the nerve root. And only then should one try to retract the nerve root medially to expose the huge disc herniation. This will help in minimizing the nerve root trauma due to retraction of the nerve root to expose the disc bulge.
Advantages of the Modified Knee-Chest Position— Dr Rohidas’s Knee-Chest Position—Vajrasana/Namaj Position
- No need of any costly frames or spinal attachments.
- Simple position
- Simple operating table can be used for this position
- No need of induced hypotension for venous oozing. As the head is lower than caudal end, due to gravity venous drainage is toward the heart
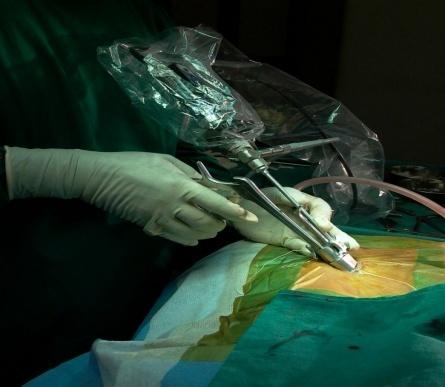
The incision is in paramedian position around 10 mm from midline. Fascia is cut also in paramedian position and then muscles are separated off midline, from spinous process and interspinous ligament. Adequate separation of muscle from spinous process and interspinous ligament is the key to prevent muscles intruding in to outer tube. Muscle intruding in to the outer tube is one of the initial problems in learning curve with Endospine. Osteotome available in Endospine set, is used to achieve subperiosteal dissection of muscle from lamina. Then the outer tube is fixed in between the retracted muscle laterally and spinous process medially. The incision should be of adequate length so that the outer tube is snuggly fixed. So that the stability as well as the mobility of endospine is not compromised. Then the inner tube is inserted in to outer tube. When the localization is correct, surgeon should see the lamina in the cranial part of outer tube and the interlaminar window in caudal part.
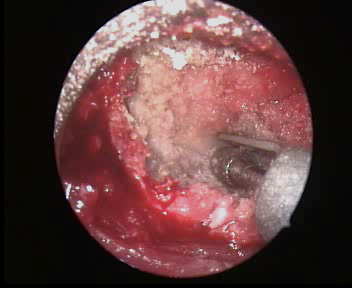
Excision of lamina
Excision of lamina is carried with 3 mm bite, 45 degree Kerrison punch. To start with we have to start at the base of spinolaminar junction. This is the area where the dura is away from lamina and there are less chances of injuring dura with Kerrison punch. Then the excision is continued laterally and cranially till the anteroinferior attachment of ligament flavum to lamina is detached. One can use up bite curette to detach the flavum from lamina. Especially at L5/S1 level where the interlaminar window is quite wide and we want to preserve the lamina, use of curette is advisable. Use of curette is advisable in previously operated cases, where already there is an open laminectomy associated with thick previous surgery scar. Curette is used to detach scar from remaining part of lamina. Initially in the learning curve, it is advisable to remove part of lamina so that the flavum attachment is detached from lamina. So that the flavum can be detached easily and pulled caudally. Later on, after sufficient experience one can remove part of lamina and detach flavum. So while decompressing the traversing root if one needs more excision of lamina, it can be excised, so as to decompress the traversing root adequately. It means adequate excision of lamina has to be the goal for adequate decompression of traversing root. It is easy to remove lamina while operating a Lt. sided disc herniation from Lt. side approach. It is difficult to take the first bite of lamina while operating from Rt. side for a right sided disc herniation. For right sided approach it is advisable to take bite of bone with Kerrison punch at base of spinous process at spinolaminar junction. Once part of lamina is excised then Kerrison punch is rotated in such a way that it can be used as backward cutting Kerrison punch. In the learning curve one can use a separate backward cutting Kerrison punch. But to move or push the whole endospine with backward Kerrison punch will be little difficult than using upward cutting punch by rotating it, as it will be in the same axis of push.


The amount of lamina to be excised also depend upon the type of disc herniation and also the lumbar disc level to be operated. In lumbar region the interlaminar distance and interpedicular distance becomes narrow as we go from caudal level ie. L5 / S1 to cranial level ie. L1 / L2. Hence we may not have to remove lamina at L5 / S1 level, in most of the cases, as the interlaminar window is quite wide, but at L4/5 level we may have to remove part of lamina quite often. As we go for the higher level we definitely have to remove significant part of lamina. This also depends upon sacralisation of L5 vertebra or lumbarisation of sacral vertebra or partial sacralisation of L5. In case of a central large disc herniation for the adequate decompression of traversing nerve root, we mostly have to remove significant part of lamina. Because the nerve root and dural sac is severely stretched over large disc bulge / large extruded disc. In an extruded and superiorly migrated disc significant part of cranial lamina has to be removed so as to expose and then pull down easily the superiorly migrated disc fragment. This will prevent inadequate removal of superiorly migrated disc fragment. For an extruded and inferiorly migrated disc part of caudal lamina has to be removed for complete removal of inferiorly migrated disc.
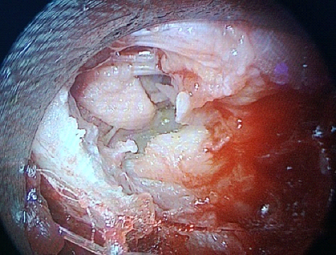
Excision of ligamentum flavum

Once the flavum is detached from the anteroinferior attachment to lamina, it is retracted caudally from lamina. One can see the sky blue coloured dural tube. To protect the dural tube it is advisable to push a cottonoid under ligamentum flavum and over dural tube, in to epidural space. This cottonoid will push the dura anteriorly. Flavum is removed with 3 mm bite, 90 degree Kerrison punch. There is a trick while excising the flavum. We have to hold the flavum with Kerrison punch, after holding it pull it little bit upwards and then take a bite so that there are less chances of duramater getting caught with the Kerrison punch bite.
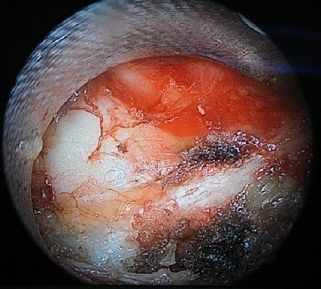
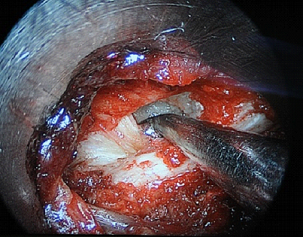
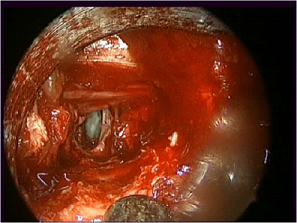
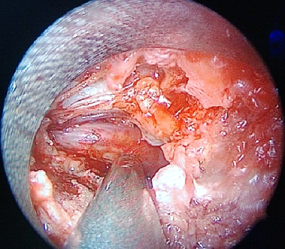
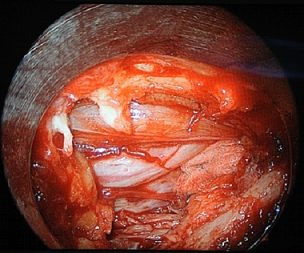
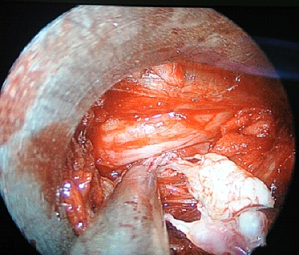
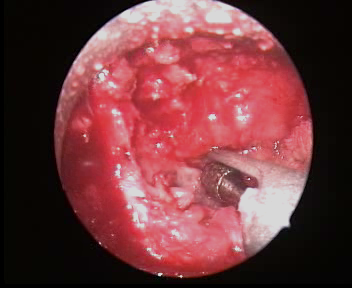
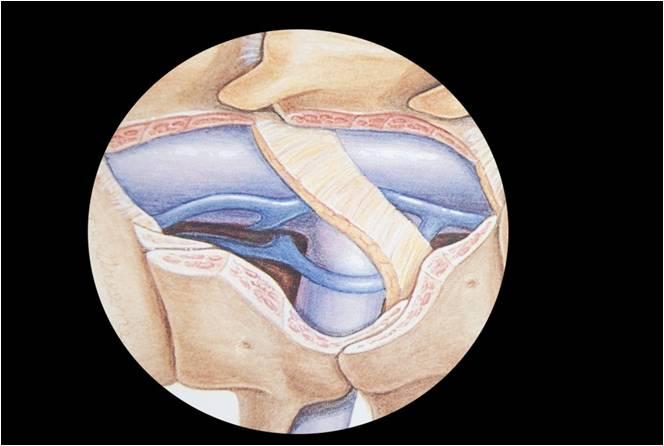
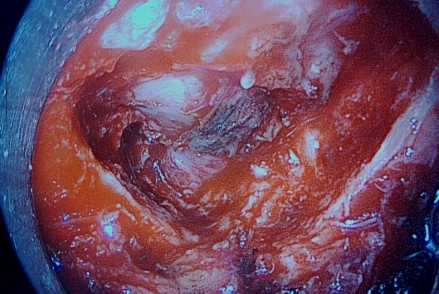
Decompression of traversing root
Laterally the flavum attachment to medial facet is cut with Kerrison punch. Then medial facet is undercut so that the traversing root is decompressed. While undercutting medial facet a 3 mm bite, 45 degree Kerrison punch is placed in between the traversing root lateral edge and medial facet, and then turned / rotated in such a way that the cutting edge of Kerrison punch is moved away from nerve root. At the same time non cutting edge of the Kerrison punch will retract the traversing nerve root medially away from medial facet, while cutting the hypertrophied medial facet. Adequate decompression of the traversing root has to be achieved. Adequate nerve root decompression means one has to see the shoulder of the nerve root, axilla of the nerve root and the nerve root passing in to the neural foramen. For this we might have to remove part of superior articular process of caudal vertebra forming the roof of neural foramen. Also cranial part of caudal vertebral lamina has to be removed to deroof the nerve in the foramen. If a large extruded disc fragment is present, then it is easy to perform foraminotomy after the extruded disc fragment is removed. Relaxed nerve root will help surgeon to perform foraminotomy safely and easily.
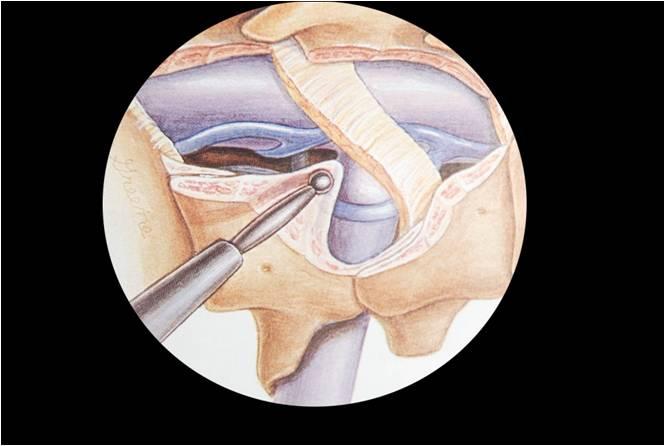
Retraction of traversing nerve root
The traversing nerve root needs adequate decompression. The meaning of adequate nerve root decompression is, we should be able to see the shoulder, axilla of the nerve root and root passing in to the neural foramen. Adequate nerve root decompression is necessary for less traumatic retraction of the nerve root. Extent of adequate decompression will be different for a simple lateral disc herniation and for a central large disc herniation, and also disc herniation with bony canal stenosis. Then we have to push a cottonoid over shoulder of the nerve root, which will retract / push the shoulder of nerve root medially. After this another cottonoid is pushed caudally so that the nerve root is retracted medially to expose disc space / annulus. After pushing the first cottonoid over shoulder of nerve root, nerve root is retracted medially to expose annulus. This will provide space lateral to the nerve root, so that Kerrison punch can be used to undercut medial facet. One should be careful while pushing cottonoid. The tip of cottonoid should be always be under vision. We should not push one cottonoid over another, as it will be difficult to trace the first cottonoid pushed away by the second cottonoid. The cottonoids are used without thread.
One has to be cautious while using cottonoid in extruded migrated disc. If the extruded disc is superiorly migrated then one should not use cottonoid over shoulder of the nerve root and vice versa same for inferiorly migrated extruded disc for caudal cottonoid. As this might push the extruded sequestrated migrated disc fragment away from the approach area, / visual field underneath lamina. After retraction of the nerve root if there are any epidural veins seen then we can use endoscopic bipolar to cauterize veins. With the knee chest position which author Dr. S. M. Rohidas uses, in most of the cases epidural veins does not create inconivence. In very few cases Authour Dr. S. M. Rohidas has to use endoscopic bipolar cautery. There is an in built nerve root retractor in Endospine. One should be cautious while using nerve root retractor. Nerve root needs to be adequately decompressed. While using nerve root retractor we use three instruments at a time, the suction, instrument through working channel and the third instrument the nerve root retractor. Endospine is a mobile system, means it can be moved in any direction. But while using nerve root retractor we have to keep the Endopsine system stable. Because if the endospine is not stable while using nerve root retractor, then there are chances of damage to the retracted nerve root because of aggressive rubbing of nerve root retractor. If the nerve root is not adequately decompressed then, with mobile Endospine, nerve root damage will be still more. Hence in initial learning curve we would like to advise not to use nerve root retractor in initial few cases. In comparison with fixed endoscopic technique or microscopic technique mobile endospine system has disadvantage of using nerve root retractor. In microscopic technique assistant can use angled nerve root retractor to retract the nerve root, which is not moving with the two instruments of the operating surgeon. Same is true with fixed tubular retractor system. Rarely one can find conjoint nerve roots which can create difficulty in dissection of the lateral edge of the nerve roots.
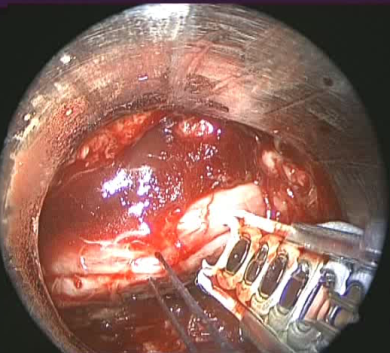
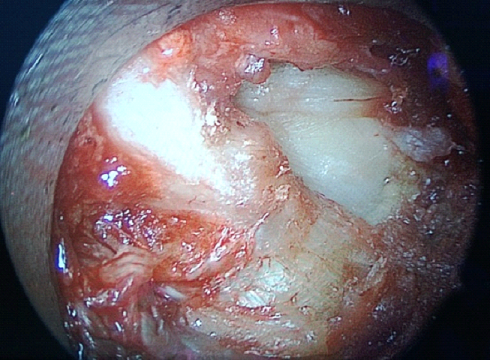
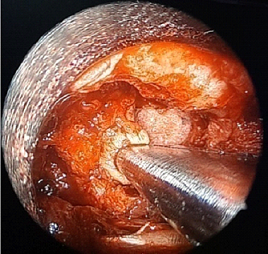
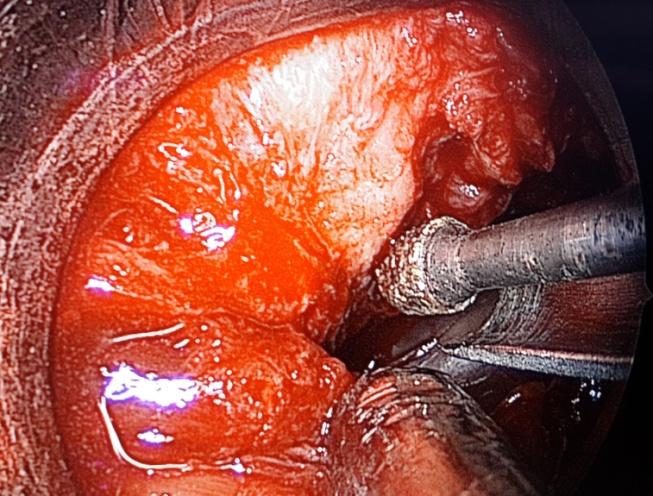
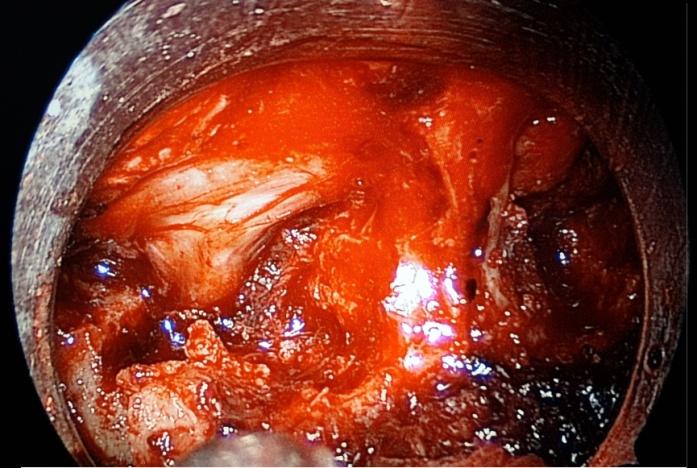
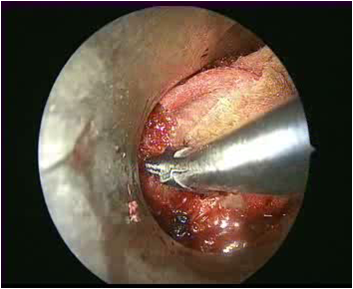
Endoscopic Discectomy
Once the annulus is exposed we may see annular tear through which the degenerated nucleus pulposus is herniating. The same annular tear can be enlarged so as to enter the disc space. First the extruded fragment is removed and then the contained part of the degenerated disc is removed. We do not advoacate aggressive discectomy for fear of damage to end plates. But it should not be compromised or inadequate discectomy. We have to use discectomy forceps in a particular method / way. After introducing the disc forceps through the annular opening we should angulate the whole endospine system to opposite side, so as to reach the opposite far lateral end as much as possible. And after angulating the system with disc forceps we have to open the disc forceps to excise the degenerated disc. ( 2 ).
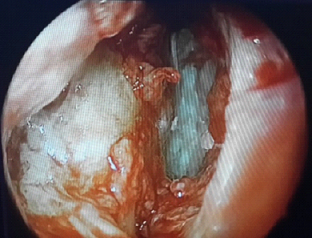
We can use endoscope to inspect the disc space. Endoscope can be put from the working channel and then directed under vision in to the disc space. Also saline is pushed in to the disc space with 10 cc syring and annulotome. We should be able to irrigate the discectomy cavity easily so as to aspirate the irrigated saline. This we consider the end point of adequate discectomy. If the annulus is intact but still bulging significantly then we can use annulotome to puncture annulus. A 15 mm knife blade can also be used to open annulus.
Advantages of Endoscopic discectomy with Destandau’s technique
- Endospine allows the same access port and the same surgical technique to be used on vertebral disc and canal at the same time reduction in the skin incision and overall access por.
- The approach anatomy is not foreign to surgeon
- Approach does not changes according to the anatomy & vertebral level
- Magnified 3 D vision if 3 D endoscope is used hence there is no loss of depth appreciation
Management of Basic complications
Dural Injury -
CSF leak tends to occur more often during the early part of the learning curve. In initial stages, usually for a large dural defect, primary closure should be attempted. However, it is often difficult to close durotomy primarily through the outer tube. If possible, sealing off defect with a piece of the muscle and then use of fibrin glue is the best option. If this option is not available, conversion to open is the easiest way to tackle large dural defects. For the more common, small, pinhole leaks, plugging the pinhole with the muscle is sufficient. The clinical effects seem to be less malignant due to small incision and easy approximation of the separated retracted muscles over the operative area. The patient’s head is kept low immediately postoperatively and after being mobilized, as tolerated. There is no need of any lumbar drainage at .
Epidural bleeding -
Good visualization of the operative field with HD camera is essential to use Endospine. Blood can obscure the visual field. Author injects 10 ml of Xylocaine with adrenaline over the lamina with help of spinal needle before incision. This helps in hemostasis and good clean operative field. Endoscopic bipolar can be used to cauterize epidural veins after retracting decompressed nerve root. Also, in the initial bony excision, we keep the working insert with endoscope in proximal position so that lens of endoscope remains clean. Once the bone is excised with flavum, we create more space and then working insert with endoscope can be pushed to distal position for magnified view. This is inherent natural telescoping effect in between the outer tube and the working insert which is available only in Endospine-Destandau’s Technique
References
Destandau J : A special device for endoscopic surgery of the lumbar spine. Neurol Res 21 : 39-42, 1999.
Jean Destandau. Endoscopically assisted Lumbar microdiscectomy. J Minimally invasive Spinal technique. 2001, Volume 1, (1): 41-43.
Introduction
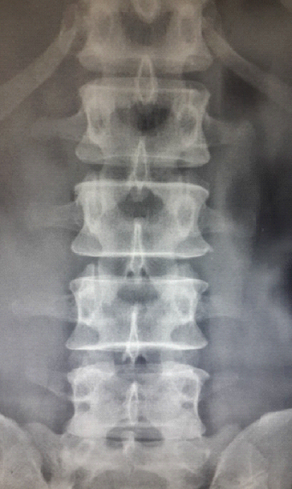
Degenerative lumbar canal stenosis ( LSS ) , is one of the most common disease of the spine that affects elderly population. Number of elderly population is increasing now a days, even in developing countries. The syndrome is the result of multiple degenerative changes that occur as the body ages. The combination of disc degeneration, facet hypertrophy, and ligamentum flavum hypertrophy leads to narrowing of the spinal canal, causing compression of neural elements.
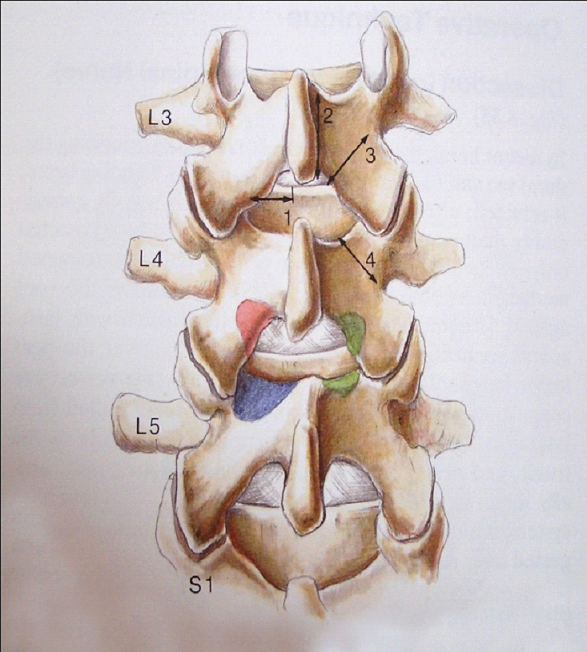
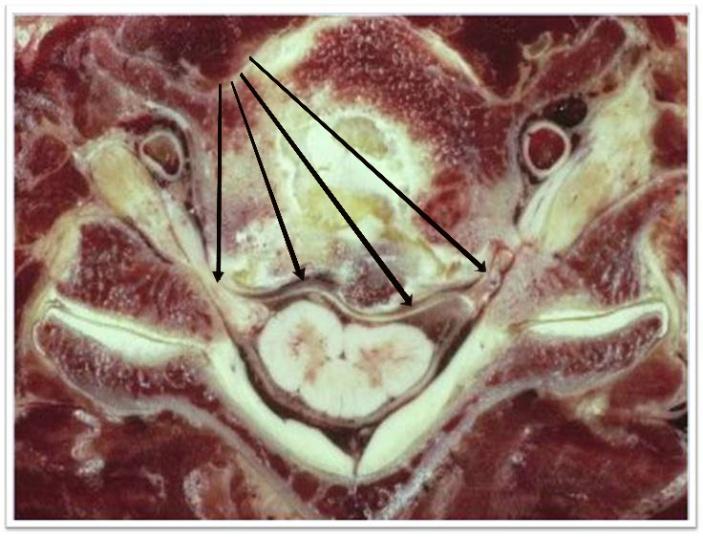
Surgical anatomy of degenerative canal stenosis
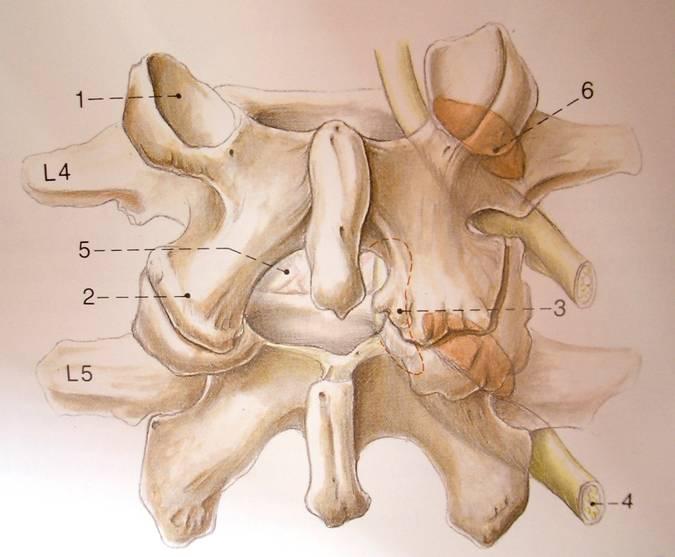
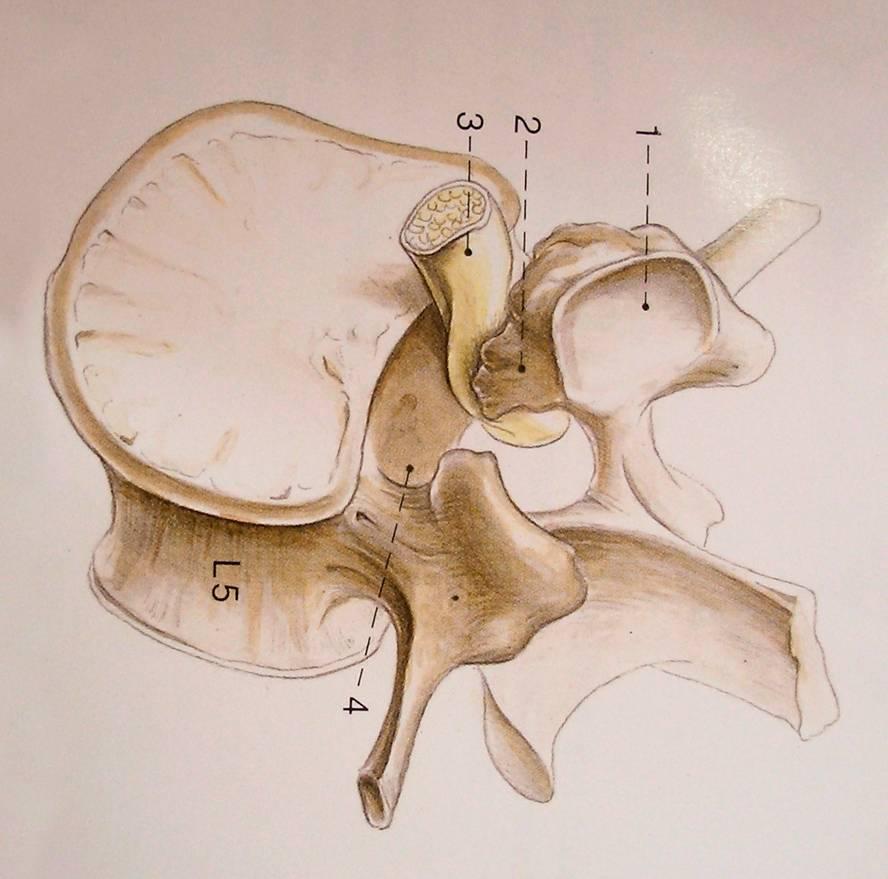
1.Superior articular process. 2. Inferior articular process. 3. Medial hypertrophied facet. 4. Traversing nerve root. 5. Interlaminar space. 6. Exiting nerve root.
Intervertebral disc blood supply is up to the age of 8 yrs only. Afterwards nutrition to the disc is provided by diffusion of fluids from vertebral body to disc and vice versa. There is rise in intradiscal pressure by sudden compression loading, which is partially minimized by transfer of fluid from disc to vertebral body. This tissue fluid transfer acts as a safety valve and thus protects the disc (1 ).
Facet joint in between the superior articular process of inferior vertebra and inferior articular process of superior vertebra is an arthroidal joint, which permits only gliding movements. Lax capsule of facet joint is reinforced by ligamentum flavum anteriorly and supraspinatous ligament posteriorly. The strong fibers of annulus prevent movements in these facet joints in young age. Now when due to wear and tear / degeneration, these annular fibers become lax / degenerate, excessive joint play is permitted at these facet joints. Hence degenerative changes within disc and annulus make these posterior joints more vulnerable to strain and hypertrophy. The facet of superior articular process forms the roof of lateral recess while it is bounded anteriorly by posterior surface of vertebral body and intervertebral disc.
The nerve root leaves the dural sac approximately at the level of intervertebral disc and the enters the lateral recess which turns in to intervertebral canal at the level of inferior margin of pedicle.
- Under pathological conditions due to ageing, wear and tear, trauma, there is increased loading of facet joints. Due to this the medial border of superior articular process develops a spondylotic scalloping. With this spondylotic scalloping – medial facet hypertrophy and added intervetrebral disc protrusion the nerve root is compressed in the lateral recess. Pathologic changes in disc & facet joint.
- Cascade of events at disc and facet joint. Aging- biochemical & mechanical changes in disc- decrease ability to withstand cyclical loading. Annular tears– loss of disc height-annular bulging—osteophyte formation.
- Degeneration facet jt. –disc height loss—increase loading on post. Facet & capsular structures- joint erosion-loss of cartilage & capsular laxity--- facet hypertrophy & osteophyte formation.
Lateral Recess Stenosis
- Osteophyte on superior articular process enlarge anteriorly & medially.
- Osteophytes form circumferentially at vertebral margins at the attachment of annulus in an attempt to autostabilize the motion segment.
- Portions of osteophytes – uncinate spurs– protrude from end plate/disc margin –lateral root entrapment.
- Disc height loss- decrease cross sectional area of NF – symptomatic
Lateral Canal Stenosis
As the pathologic changes generally are concentrated at the level of interlaminar space, focal laminotomy was the natural first step in evolution of surgical procedures for lumbar spinal stenosis. By sparing most of the lamina, spinous process, and interspinous ligamentous complex, laminotomy allowed improved post op. muscle reattachment & helped in preserving the biomedical integrity of the spine. ( 2 ).
A wide laminectomy was the traditional surgical treatment for lumbar canal stenosis. ( 10 ). Last decade has seen modifications in this with help of various minimally invasive techniques. This traditional treatment of wide laminectomy insist of an extensive resection of posterior spinal structures such as interspinous ligament, spinous process, bilateral laminae, portion of facet joint and capsule, and ligamentum flavum. This technique of wide decompressive laminectomy, medial facetectomy and bilateral foraminotomies is used for long period. May be this wide decompression has compromised the existing stability, which has encouraged surgeon to think of stabilization to overcome instability. But this extensive open decompression is associated with significant pain, long hospitalization, morbidity, prolonged recovery period and associated concominant medical complications in elderly people.
In 1993 surgical bilateral decompression laminectomy with a unilateral approach, which preserved the paravertebral muscles attachment was reported by Joson R. M. and McCormick K. J. ( 11). Then afterwards this technique of bilateral decompression with unilateral approach became minimally invasive with use of microscope. ( 12 ). This less aggressive surgical approach improve the post operative outcome. (13).
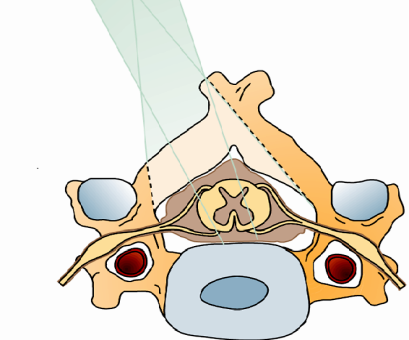
Young et al also introduced the concept of unilateral approach for performing a bilateral decompressive laminotomy in which the ipsilateral side of the canal is decompressed first and the contralateral canal, lateral recess, and intervertebral foramen are decompressed underneath the midline structures. ( 5 ). This approach had the advantage of preserving the spinous process and midline ligamentous structures. Also this approach allowed surgeon to access both sides of spinal canal exactly where the compression is maximum. ( 6 ).
Indications – Degenerative lumbar canal stenosis with neurogenic claudication, with or without disc herniation. Multilevel lumbar canal stenosis.
Contraindications - Severe instability.
Position, Localisation and incision.
Authour Dr. S. M. Rohidas uses knee chest position. Knee chest position which we use gives completely lax abdomen in between both thighs along with interspinous distraction. This helps in opening the interlaminar window in severe stenosis along with relatively less epidural oozing while approaching through same 15 to 18 mm incision. Exact localization is done with help of localizing pin and c arm. As in some of the canal stenosis cases there is no significant disc herniation, it is always helpful / advisable to reconfirm the level with the c arm after fixing the outer tube. This will prevent wrong level surgery. The incision is paramedian around 10 to 15 mm from midline. The incision is relatively lateral as compared to simple discectomy because we have to angulate the endospine system so as to reach the opposite side underneath the spinous process. If the incision is too close to the midline, then there are chances of fracture at spinolaminar junction due to excessive pressure put while angulation, in osteoporotic patients.
Technique -
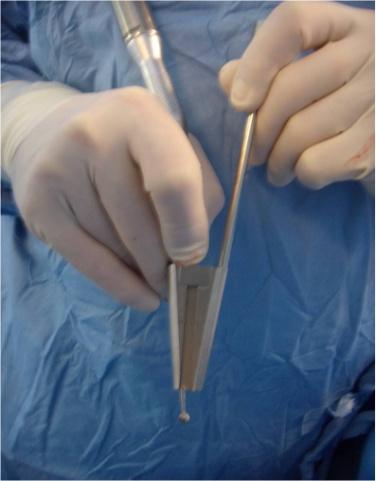
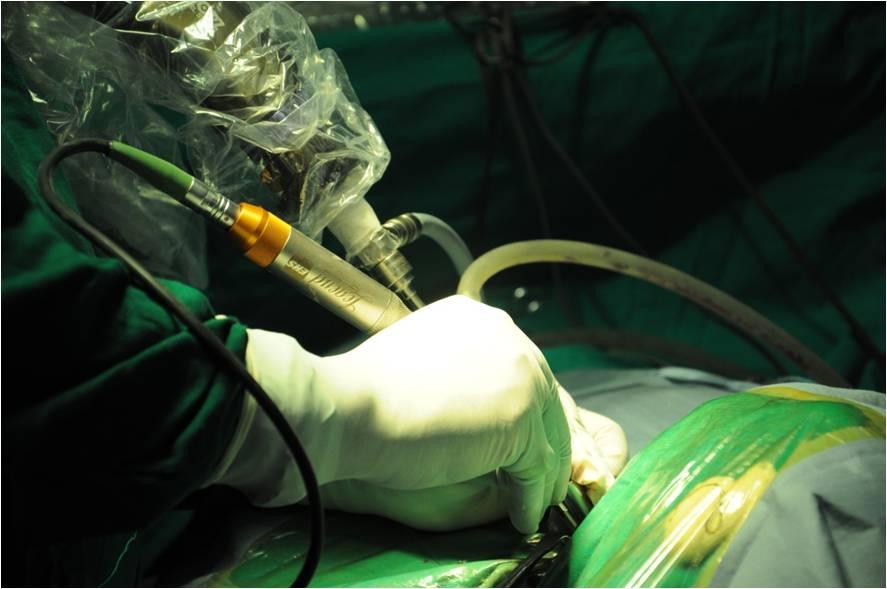
Once the outer tube is in place, it is advisable to reconfirm the level again at least in initial learning curve. Because in canal stenosis disc bulge may not be there in all cases to confirm the level. Excision of lamina started through the interlaminar window. If there is no interlaminar window then one can use endoscopic drill, 3 mm tip, to thin out the lamina bone. The pencil grip drill is supported over the edge of working channel and used in transverse plane, so that the drill will not drop down accidently. In fact endospine helps to get control of drill with mobility and stability.
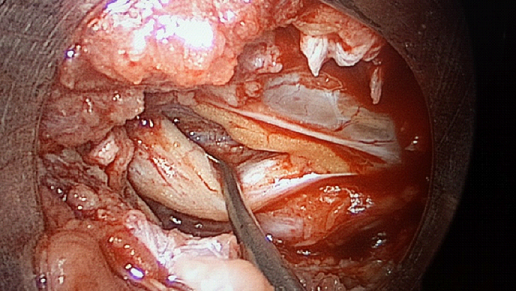
Significant part of cranial lamina excised to detach the inelastic, infolded flavum. Then adequate size cottonoid is pushed in front of flavum to push dura anteriorly. This helps in preventing dural tear or accidental punctures. Laterally the medial facet is undercut with removal of flavum so as to see the lateral edge of dura, and nerve root. From the lateral dural margin, nerve root is followed caudally till neural foramen. The caudal attachment of flavum to cranial part of caudal lamina is detached and then followed medially. Whole endospine system with instrument, endoscope and suction can be angulated medially. First the base of the spinous process is undercut with Kerrison punch to reach opposite side. If the base of spinous process is too thick then drill is used to remove bone. Dr. S. M. Rohidas the authour uses special endoscopic drill which has a protection sheath. The tongue like protection sheath protects the dura and can be used to press dura anteriorly / down, over a cottonoid.

Once adequate space is created by undercutting the base of spinous process, endospine is angulated medially by 30 to 45 degrees, that the outer tube is supported under the base of spinous process and interspinous ligament. This gives tangential view of the opposite spinal canal, and lateral recess. Kerrison punch is used to undercut the opposite lamina so as to detach the flavum attachment. The lateral edge of dura of opposite side is then identified. A small cottonoid is passed over the lateral dural edge / shoulder of traversing nerve root, cranially which will retract the dura, and shoulder of nerve root medially. This will provide working space lateral to nerve root. Lateral dural edge is followed caudally so as to decompress the traversing root till neural foramen. One of the advantages of this technique is that the cutting edge of the Kerrison punch is always away from the dura and nerve root. The same is true for endoscopic drill with tongue like protection sheath. ( 9 ).
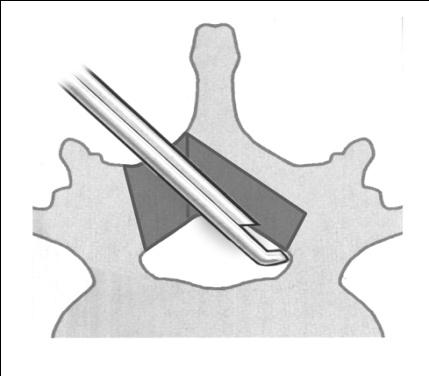
When one is efficient to use drill with Endospine, then first major bony work can be finished with drill. We start with the cranial lamina and drill the bone of lamina till the flavum is detached, then by angulating the scope medially base of spinous process is undercut. Laterally the medial facet is undercut and lateral recess is decompressed. Caudally the part of cranial part of caudal lamina is drilled to detach flavum attachment. Drilling is continued medially following the cranial part of caudal lamina to opposite side. Lastly the medial facet of opposite side is undercut over the thick flavum. Here flavum is removed after completion of bony decompression, so that during drilling of bone the flavum acts as a protection to dural tube & nerve roots

Dr. S. M. Rohidas author uses Midas Rex drill 3 mm tip with a protection sheath. The guard is placed over the flavum and cutting surface is away from dura. The tongue like projection of guard can be used to push dura anteriorly away from the cutting edge.
Drill should be used carefully. Bone dust can get sprinckled over endoscope lens. Saline irrigation is used to clean the lens. But whenever it is necessary endoscope is taken out to clean the lens so as to prevent fogging. Drill is supported over the outer tube so that it should not slip inside accidently. Rather than to and fro movements side ways movements will help in preventing this unusual complication with drill. ( 7, 8 ).
Authour Dr. S. M. Rohidas uses ultrasonic bone dissector / rasp to undercut opposite lamina and facet, in severe canal stenosis. This is more safe technique as it will not damage the soft structures like dura or nerve root, while removing the bone.
Whenever it is necessary endoscopic bipolar is used to control epidural bleeding. Adequate decompression of both sided nerve roots is confirmed by mobilizing it medially.
Canal stenosis at L5/S1 and L4/5 can be approached through single unilateral incision due to the caudal angulation of the L5/S1 disc space. Some part of L5 lamina can be kept intact for the muscle reattachment post operatively. Sometimes complete ipsilateral hemilaminectomy has to be performed. For two levels above L4/5 we have to take two separate incisions. Here also small part of cranial lamina is kept intact for muscle reattachment. ( 4 ).

Steps in bilateral canal & root decompression with unilateral approach.
- Ipsilateral lamina excision to detach flavum attachment.
- Ipsilateral medial facet undercutting to detach flavum attachment.
- Ipsilateral detachment of flavum from caudal lamina.
- Excision of ipsilateral flavum.
- Ipsilateral foraminotomy.
- Endospine angulated to opposite side. Undercutting of base of spinous process and opposite lamina to detach cranial flavum attachment.
- Over the top / over the flavum undercutting of medial facet to decompress opposite lateral recess.
- Detachment of flavum attachment from opposite side caudal lamina following from ipsilateral to opposite side.
- Removal of opposite flavum.
- Opposite / contralateral traversing root decompression with foraminotomy.
Authour Dr. S. M. Rohidas uses 10 cc of diluted Sensorcaine for infiltration in to muscle and skin. This reduces post operative incision pain significantly. Fascia and skin is closed with 3 -0 vicryl .

Advantages—
- No need of instrumentation as existing stability is not compromised.
- Even in obese patient skin incision remains small, unlike open or microscopic approach, where the length of incision is directly proportional to the depth of lamina from skin.
- Intraspinal procedure / underneath the base of spinous process, mobile vision of opposite lateral recess is significantly better as compared to other approaches with mobility of Endospine. Every time there is no need to fix the system and or change the focus of microscope / endoscope.
Conclusion
Endoscopic bilateral root decompression with canal decompression with unilateral approach is a safe and effective alternative treatment to classic laminectomy open techniques. Operative time is disadvantage in initial learning curve. The steep learning curve is because of following things. (1). Learning of getting 3 D appreciation with a 2 D high definition vision. (2). Difficult hand eye coordination with mobile Endospine system. And (3). Narrow corridor / working space through Endospine. In experienced hands this approach provides less blood loss with preservation of existing stability. This helps in early mobilization in post operative period which is a real issue in elderly medically compromised patients who present with canal stenosis.
References
Microsurgical anatomy of lumbar stenosis- Hans- Jorgen Reulen MD. Adolf Muller MD. Neurosurgery -39:345-351-1996.
Arynapur and Ducker in their description of multilevel laminotomies reported a longitudinal good outcome rate of 79% to 85% at 2 yr. follow up. Neurosurgery 26:429-433, 1990.
Khoo LT, Khoo KM, Isaacs RE, et al. Endoscopic lumbar laminotomy for stenosis. In Perez-Cruet MJ, Fessler RG, eds. Outpatient Spinal surgery. St. Louis : Quality medical publishing, 2002, pp 197-215.
Lin PM. Internal decompression for multiple levels of lumbar spinal stenosis: A technical note. Neurosurgery 11: 546-549; 1982.
Young S, Veerapen R, O’ Laoire SA. Relief of lumbar canal stenosis using multilevel subarticular fenestrations as an alternative to wide laminectomy: Preliminary report. Neurosurgery 23: 628-633; 1988.
Wada K, Sairyo Sakai T, Yasui N. Minimally invasive endoscopic bilateral decompression with unilateral approach ( endo_BIDUA ) for elderly patients with lumbar canal stenosis. Minimally invasive Neurosurgery 2010: 53(2):65-68.
Ikuta K, Tono O, Tanaka T, et al. Surgical complications of microendoscopic procedures for lumbar spinal stenosis. Minimally invasive Neurosurgery 2010: 50(3):145-149.
Sairyo K, Sakai T, Higashino K, Inoue M, Yasui N, Dezawa A. Complications of endosopic lumbar decompression surgery. Minimally invasive Neurosurgery 2010: 53 (4): 175-178.
Yoshimoto M, Takebayashi T, Kawaguchi S, et al. Minimally invasive technique for decompression lumbar foraminal stenosis using a spinal microendoscope: technical note. Minimally invasive neurosurgery 2011: 54 (3 ): 142-146.
Postacchini F. Spine update : Surgical management of lumbar spinal stenosis. Spine 1999; 24: 1043-1047.
Joson RM, McCormick KJ. Preservation of supraspinatous ligament for spinal stenosis. A technical note. Neurosurgery 1993; 21: 420-422.
McCulloch JA. Microsurgical Spinal Laminotomies In; Adult Spine; Principles and Practice. JW Frymoyer, ed. New York; Raven Press Ltd: 1991.
Podichetty VK, Spears J, Isaacs RE et al. Complications associated with minimally invasive decompression for lumbar spinal stenosis. J Spinal Disord Tech 2006; 19: 161-166.
Introduction
The popularity of different operative techniques for the treatment of postarolateral disc herniations has changed according to different neurosurgical schools of thought. Early 1950’s Cloward first described his success with treating cervical disease through an anterior approach. ( 1 ).
His techniques received luckwarm reception form neurosurgical community as posterior approach was the current fashion. Attractive features of the anterior approach include a small neck scar, minimal muscle damage, less postoperative pain & muscle spasm, and shorter hospital stay. Over last two decades enthusiasum for anterior approach was so strong that neurosurgical generation was less familiar with posterior foraminotomy as an operative technique.
The effectiveness of posterior cervical laminoforamonitomy for decompression of lateral recess and neural foramen is well documented in numerous publications. ( 2, 3 ). When compared with standard anterior cervical approach, the posterior approach via “keyhole” may provide better exposure for decompression of exiting nerve root removal of lateral discs. ( 4 ).Their work has shown that adequate foraminal exposure can be achieved without destroying the facet joint. As long as less than 50 % of facets are removed there is little compromise of biomechanical strength of cervical spine. ( 5 ). The posterior approach avoids risks of injury to the anterior structures of neck, like trachea, esophagus, thyroid, thymus, carotid arteries, jugular veins, vagus nerve, recurrent laryngeal nerve, superior laryngeal nerve, and thoracic duct. Also cervical laminoforaminotomy is an approach that treats the offending pathology without necessitating fusion. Various longitudinal studies now demonstrate as increased incidence of adjacent level problems following cervical fusion. ( Hunter LY, Braunstein EM, Bailey RW. Radiographic changes following anterior cervical spine fusions. Spine 5: 399-401, 1980.) ( 6 ). Hence when possible an approach avoiding arthrodesis seems particularly more relevant. Also overall no statistically significant difference in results between anterior and posterior approaches for treatment of isolated cervical compressive radiculopathy has been demonstrated. ( 7 ). The popularity of posterior laminoforaminotomy was decelerated by technical limitations, like limited surgical view, bleeding from epidural veinous plexi and bone etc. Muscle dissection is needed for adequate exposure. Contrary to anterior approach it is the only thing which needs dissection. Use of Endospine has helped in minimizing the trauma to the muscle with use of tubular retractor and also minimizing the muscle trauma with small targeted incision after exactly localizing the disc level.
Indications -
Soft unilateral disc herniation, with nerve root compression. Two consecutive unilateral disc harniations. Also posterior approach can be used for focal lateral thickening of ligamentum flavum, facet thickening with hypertrophy. Some absolute indications for posterior approach include, persistent and recurrent radiculopathy after anterior cervical discectomy and fusion. Also patients having anterior neck infection, tracheostomy or prior irradiation posterior approach will be a choice. Posterior approach is ideal for C7-T1 lateral disc herniation which is difficult to approach from anterior especially in patients with short neck.

Contraindication -Symptomatic central cervical disc herniation with myeloradiculopathy, diffuse OPLL compressing cord anteriorly, Severe instability with deformity.
Equipments-
- Silicon gel horse shoe for prone position.
- Endospine cervical set which includes 2 mm Kerrison punches.
- HD camera.
- High speed drill with 2 mm & 3 mm tips preferably pencil grip.
- Ultrasonic bone dissector optional for safe bone removal.
- C arm for localization before surgery and during surgery.
Position, localization -
We use prone position on bolsters. Sitting position can be used to get relatively clean operative field. To avoid a rare complication of air embolisum with sitting position, we always used prone position for posterior approach.

We use a separate localizing pin for cervical region based on the same principles as of lumbar localizing pin, but smaller in size. The semicircle arm of localizing pin can be moved in two different planes, so as to mark the direction of the disc space. With localizing pin and c arm the concerned disc space is exactly localized.


Surgical technique
Incision
Authour Dr. S. M. Rohidas uses 10 cc of Xylocaine with adrenaline for infiltration. The incision is around 10 – 15 mm away from midline. Length of incision depends on whether we want to target one level or two through same incision. Fascia is thick in cervical region hence it needs to be cut sharply with scissors. Fascial opening must be equal to the skin incision so that outer tube fits snuggly into it. The spinous process in cervical region is not that strong as it is in lumbar region, hence adequate fascial incision will help in fixing the outer tube. Muscles are separated off the midline, so as to expose the laminae, and facet. Bipolar cautery is used for to control bleeding from retracted muscles. we use two gauze pieces with thread for retraction of muscles . One is passed cranially and other caudally over laminae to retract muscles laterally.
Then outer tube is fixed in between muscle laterally and spinous process medially. A small retractor blade is used lateral to outer tube to retract muscle. Once again with C arm and outer tube in place, concerned disc level is again reconfirmed.
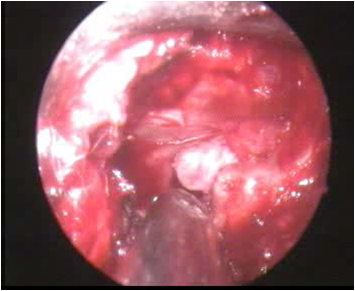
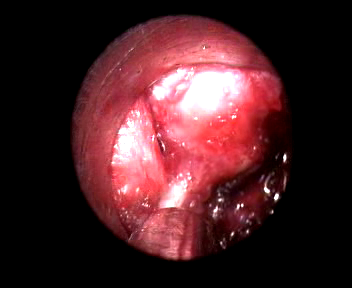
The inner tube is then fixed in to the outer tube. When endoscope is used both cranial and caudal laminae with facet are seen. In cervical region the interlaminar window is smaller as compared to lumbar region. 2 mm or 1 mm Kerrison punch is used to excise very small part of cranial and caudal lamina. Sometimes it is not necessary to remove lamina as the interlaminar window is wide and laterally we can see facet joint nicely.
Laterally the neural foramen is opened to decompress the nerve root. In cervical region often the ligamentum flavum is thinned out or sometimes absent near lateral edge of interlaminar space. Hence where the interlaminar space ends due to absence of flavum, there is high risk of iatrogenic trauma to dura or spinal cord. The bone in axilla of the nerve root is difficult to excise with Kerrison punch as it is end on. There is a fear of accidental slipping of Kerrison punch into spinal canal. Endoscopic 2 or 3 mm drill is used to remove bone in the axilla of nerve root. Sometimes lamina can be oriented in vertical fashion, which makes it difficult to bite with Kerrison punch. Authour Dr. S. M. Rohidas uses ultrasonic bone dissector for the safety purpose in these particular situations. Ultrsonic bone dissector will emulsify bone and will not damage the soft tissue like dura and nerve root.
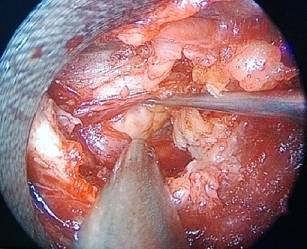
Once the nerve root from dural sleeve to the foramen in exposed, flavum is excised. Adequacy of the decompression of nerve root is confirmed by palpating the nerve root along its course with a small nerve hook. Either a nerve hook or no. 4 Penfield retractor is used to retract the nerve root superiorly and medially to expose the disc space and the concerned herniated disc fragment. To do this safely additional exposure can be obtained by drilling small portion of superomedial portion of pedicle just below the exiting nerve root. Authour Dr. S. M. RohidasI uses ultrasonic bone rasp to remove superomedial portion of pedicle, which is more safe than drill. This will create more space to mobilize the nerve root medially. Excessive unnecessary decompression of facet should be avoided to prevent iatrogenic instability of cervical motion segment. Integrity of facet joint is required for stability. 50 % facet joint should be preserved for stability. On the contrary this much resection of facet permits adequate exposure of nerve root.
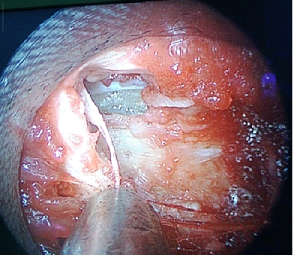
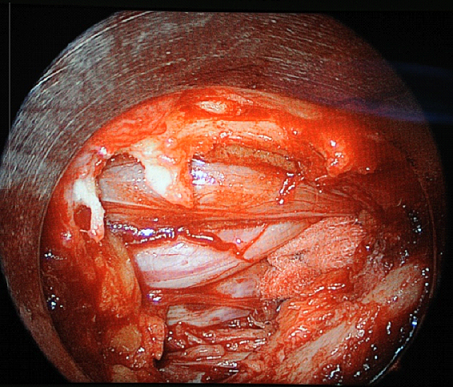
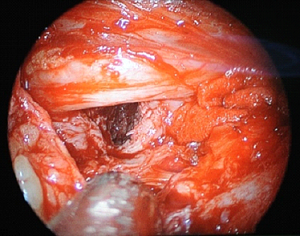
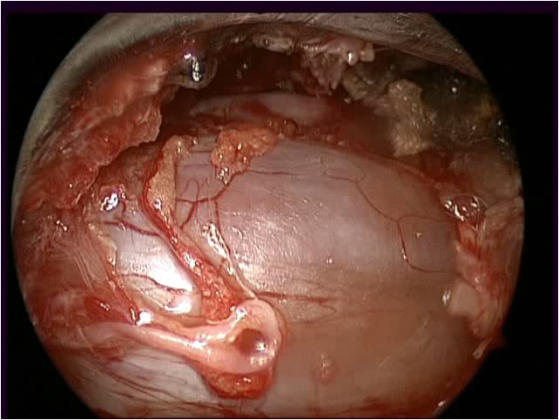
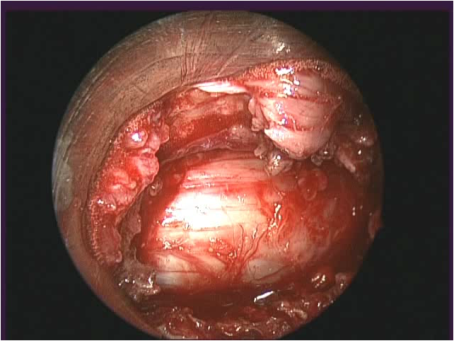
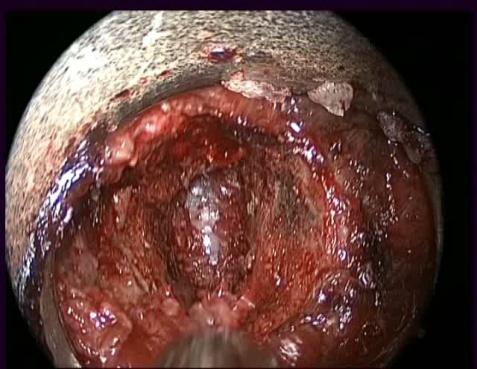
Laminoforaminotomy and decompressed nerve root
There may be some epidural oozing from the veins which can be controlled with small gelfoam or betadine hydrogen peroxide irrigation. Simple packing with cottonoid for some time also helps a lot. Rarely endoscopic bipolar might be necessary to control epidural venous bleeding. Bleeding underneath the edge of lamina is controlled with 45 degree angle endoscopic bipolar.With nerve hook disc herniation is searched in the axilla or rarely over the shoulder. Only the extruded part of the disc is removed. Once the herniated disc is removed concerned stretched nerve root will become lax. Contrary to the lumbar region excessive mobilization of decompressed nerve root should be avoided. There is no need to enter inside the disc space and remove contained disc.

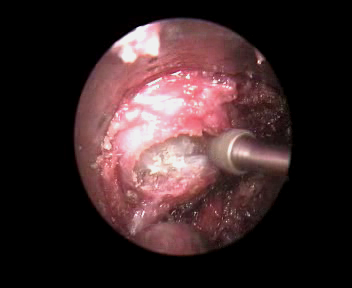
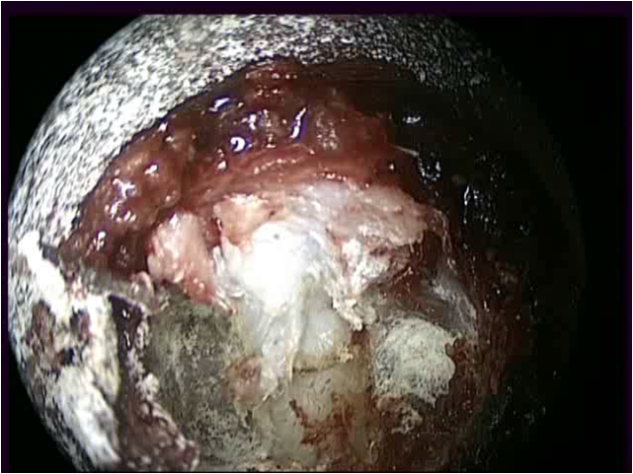
Extruded disc in axilla of nerve root
Accidental passage of nerve hook beyond the bone forming posterior margin of foramen transversarium can cause brisk epidural bleeding from venous plexus around vertebral artery.Authour Dr. S. M. Rohidas, usually places a small piece of gelfoam soaked with 40 mg of methylprednisolone over laminoforaminotomy defect for medical decongestion. Also 10 cc of sensorcaine is used to infiltrate the muscle and skin edges for postoperative wound analgesia.
Fascia and skin is closed with 2 -0 and 3- 0 vicryl respectively.
Advantages -
- Only extruded disc is removed. Rest of the disc is preserved.
- No compromise of existing stability.
- Motion segment is preserved.
Precautions -
- Preserve at least 50 % of facet joint.
- Avoid use of cautery over nerve root and dura. Simple packing for few minutes will help.
- Take extra care while removing superomedial portion of caudal vertebral pedicle to get extra space in axilla of nerve root.
Conclusion-
Posterior cervical endoscopic discectomy with endospine offers benefits of preservation of motion segment, decreased blood loss and hospital stay. This approach is not foreign as the anatomic landmarks are the same as in open posterior approach. The pain relief is immediate with relatively less post operative paraspinal muscle spasm. Early mobilization is possible with no need of cervical collar.
Posterior endoscopic cervical canal decompression bilateral decompression with unilateral approach.
Indications-
Degenerative cervical canal stenosis leading to compressive myeloradiculopathy.
Contraindications
Cervical spinal instability.
Position, localization and incision. –
We use prone position on bolsters. Localisation of disc level is done with cervical localizing pin and C arm. The incision is paramedian. The side of approach is the side which is more symptomatic or side of radiculopathy for foraminotomy. When the symptoms are equal on both sides then Lt. sided approach is preferred. Through a single incision three consecutive levels can be approached. For example to approach C4/5/6, the incision is centered on C5 and then by angulating cranially C4, and by angulating caudally C6 can be approached. For C3 to C7 compressive myelopathy with two separate incisions C3 to C7 hemilaminectomy can be achieved.

Two incisions for C3 to C7 hemilaminectomy Canal decompression for myelopathy.
Technique-
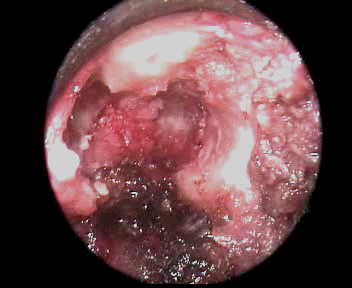
The incision is paramedian, around 1.5 cms lateral to midline so that the endospine system can be angulated to opposite side easily. Fascia is cervical region is tough, hence cut sharply with scissors. Adequate fascial opening is mandatory so that the outer tube snuggly fits in between muscle and spinous process. If the fascial incision is wide then small retractor can be used lateral to outer tube so as to retract muscle. Excision of lamina started where the interlaminar space is wide. Excision is started from caudal end of lamina as it is easy to pass Kerrison punch caudally usually. The attachment of flavum to cranial part of lamina is relatively tight hence 1 mm Kerrison punch can be used. Excision of lamina is achieved from base of spinous process, to laterally till lateral edge of dura is seen. The flavum is kept intact while excision of laimnae which acts as a protection for dura during laminectomy. Then the flavum is excised with through cut punch or 2 mm, 90 degree Kerrison punch. Flavum is not pulled while excision as this will tear epidural veins which will have troublesome epidural bleeding. For haemostasis endoscopic bipolar cautery is used.
Endospine system with scope is then angulated medially to approach opposite side. Base of the spinous process is undercut with endoscopic drill with a protection sheath to avoid dural trauma. Once sufficient space is created then opposite lamina is also undercut with drill over flavum. Here flavum is kept intact which protects dura and cord. To use Kerrison punch it is relatively difficult as there is no sufficient space in between lamina and cord. Then the flavum is excised. The cord from ipsilateral edge to contralateral edge is adequately decompressed. I use ultrasonic bone dissector in this narrow corridor for more safe surgery. Fear of slipping or kicking back of drill is not encountered while using ultrasonic bone dissector.When it is required ipsilateralforaminotomy can be performed when ever there is compressive radiculopathy along with compressive myelopathy.

The operative field is cleaned with saline and haemostasis achieved with bipolar cautery, and bony oozing with bone wax.After dural decompression small piece of gelfoam soaked with methylprednisolone is kept over dura for medical decongestion. Muscle and skin is closed with 2 -0 vicryl in layers.
Conclusion
Posterior endoscopic discectomy, laminoforaminotomy, and canal decompression provides advantage of less hospital stay, significantly less post operative pain, with preservation of stable motion segment. The efficacy is equivalent to open procedures. The posterior techniques are patient friendly also.
References
Cloward RB, Complications of anterior cervical disc operationand their treatment. Surgery 69: 175-182,1971) (Cloward RB. The anterior approach for removal of ruptured cervical discs. J. Neurosurgery 15:602-617, 1958).
Henderson CM, Hennessy RG, Shuey HM, Shackelford EG. Posterolateralforaminotomy as an exclusive operative technique for cervical radiculopathy: A review of 846 consecutively operated cases, Neurosurgery 13: 504-521, 1983.),
Zeidman SM, Ducker TB. Posterior cervical laminoforaminotomy for radiculopathy: review of 172 cases. Neurosurgery 33: 356-362, 1993.
Roh SW, Kim DH, Cardoso AC, Fessler RG. Endoscopic foraminotomy using MED system in cadaveric specimens.Spine 25: 260-264, 2000.
Raynor RB, Pugh J, Shapiro I. Cervical facetectomy and the effect on spine strength. J Neurosurgery 63: 278-282, 1985.
Olsewaski JM, Garvey TA, Schendel MJ. Biomechanical analysis of facet and graft loading in a Smith Robinson type cervical spine model.Spine 19:2540-2544, 1994.
Dillin W, Booth R, Cuckler J, alderston R, Simeone F, Rothman r. Cervical radiculopathy: A review. Spine 11: 988-991, 1986.
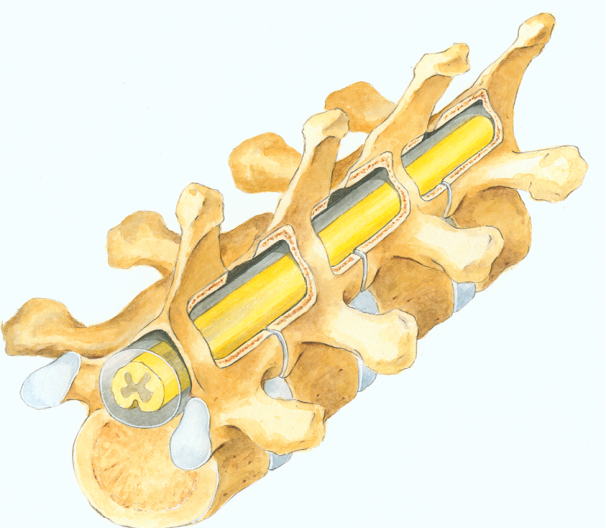
Introduction
Degenerative changes in vertebrae and intervertebral discs occur due to wear and tear from constant use of the spine along and other reasons accelerating the degeneration at the spine. Two main consequences follow. One is compression of the neural structures and the other is increased motion at the joints between the vertebrae. Neural compression may occur with or without instability at the motion segment.
Compression of nerve root (compressive radiculopathy) or spinal cord (compressive myelopathy) necessitates surgical treatment to create space for the root or cord. However these surgical procedures for decompression should not compromise the stability of the motion segment. Endospine enables endoscopic decompression of cervical nerve roots and spinal cord.
Dr. Jho described in 1996 microscopic anterior cervical foraminotomy where the transverse processes and uncovertebral joints were exposed and the decompression was performed with gradual removal of the uncinate process so as to reach the nerve root. ( 1,2)
Surgical Indications
In young patients compression of roots and spinal cord is often due to soft disc herniation whilst in the elderly the compression is due to osteophytes, hard discs, and hard, thickened posterior longitudinal ligament.
Endospine can be used for anterior endoscopic cervical foraminotomy and partial vertebrectomy as described by Jho. This is indicated for soft or hard foraminal disc herniations. In elderly patients the compressing disc is thin and hard. In such cases anterior endoscopic foraminotomy can be easily extended to the midline or opposite side where the foramen begins. (3, 4, 5).

Technique
Authors use the straight rigid, 0 degree, 18 cm, endoscope with Endospine together with endoscopic high definition (HD) camera, endoscopic drill with 2mm and 3 mm tip burs, Ultrasonic bone dissector and endoscopic bipolar cautery. The rest of the instruments such as 2mm Kerrison punch, angled (45 degree and 90 degree angles), nerve hook, Penfield dissector no. 4, and scissors are similar to those used in conventional cervical spine surgery. Bone removal is carried out through the working channel of Endospine using 3mm and 2 mm cutting high speed drill. Ultrasonic bone dissector is used to remove bone near vertebral artery, nerve root and cervical cord so as to protect these important structures. Ultrasonic bone dissector emulsifies bone and does not damage adjacent vital structures.
Positioning the patient
All operations are performed under general anaesthesia through an endotracheal tube. Patient positioning is similar to that during conventional anterior cervical discectomy. The head and neck are kept in the neutral position, without turning to the opposite side. Where the patient has a short neck, I use bilateral traction to pull the shoulders caudally. In such patients I may also extend the neck a little. Careful positioning of the neck is important to prevent injury to cervical cord and aggravation of symptoms.
Use of pin for localization

Exact localisation of the disc level is crucial in minimising tissue trauma during endoscopic anterior cervical surgery. The special localising pin used by me can be moved in three spatial planes. After localising the level of the diseased disc I obtain a precise entry point and the direction of the disc space. This facilitates foraminotomy in the antero-posterior direction to reach the nerve root and cord. In addition to the localisation of disc space using the pin, I confirm the level of the diseased disc with the help of C-arm image intensifier after exposure of disc space before starting removal of bone.


Skin incision
I use a horizontal incision similar to that used during the open cervical approach. The incision is approximately one third lateral and two third medial to the sterno-cleido-mastoid muscle at the level of the diseased disc. The platysma is cut and a space created by gentle dissection between the carotid artery –jugular vein laterally and trachea –oesophagus medially. The anterior surface of the cervical spine is exposed. At this step the transverse processes can be palpated under the longus colli muscles. The C6 transverse process can be easily identified with the help of the carotid tubercle. Two thin blades of the cervical retractor are used to retract carotid artery – jugular vein laterally and trachea – oesophagus medially. The outer tube of the Endospine with obturator is placed in the space opened up by the retractor blades. The blades of cervical retractor system are used without the holding arms of retractor. Through the outer tube, scissors are used to cut 1 – 2 mm. of the medial part of longus colli. This helps prevent injury to the sympathetic chain that is located laterally. The disc space and the uncovertebral joints can now be exposed.

Endoscopic foraminotomy
The insert with 4 mm. rigid telescope is now introduced through the working channel of the Endospine. The disc space, uncovertebral joints and base of transverse process of cranial and caudal vertebrae are defined using HD television.
The working area for the surgeon is in between the two transverse processes and medial to vertebral artery. The exiting root leaving the dural sleeve and reaching the vertebral artery measures approximately 6mm. Bone removal is performed using pencil-grip high speed drill with 2mm or 3mm cutting/diamond bits. A bone window measuring approximately 8 to 10 mm in craniocaudal direction and 5 to 8 mm in tranverse direction is created. Part of the disc medial to the uncovertebral joint is removed in the process. The endospine with endoscope is used at an angle of 15 to 30 degrees to reach the lateral parts of the disc. I follow the disc laterally and cranially to reach the uncovertebral joint. While widening this bony window I drill out the osteophytes from cranial and caudal vertebral bodies. This opens the neural foramen.I usually find the soft herniated disc at the medial part of the neural foramen. The nerve root is exposed and decompressed from the lateral edge of dural sac up to the vertebral artery. This tunnel is approximately 6 mm in diameter and follows the oblique direction of the nerve root. The intervertebral foramen in front of the nerve root is thus widened.
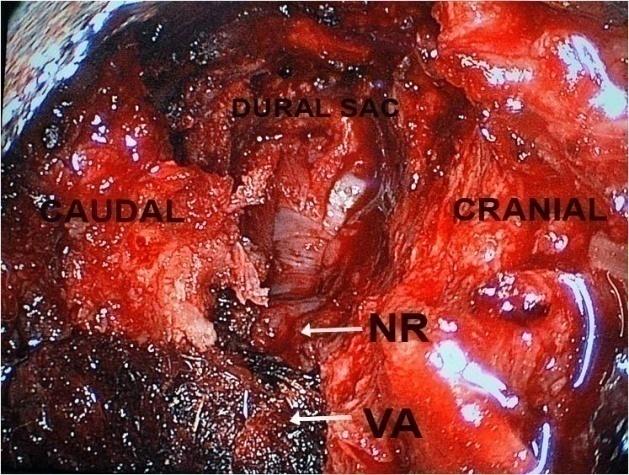
Left C4/5 foraminotomy and decompression of nerve root.NR = nerve root. VA = vertebral artery
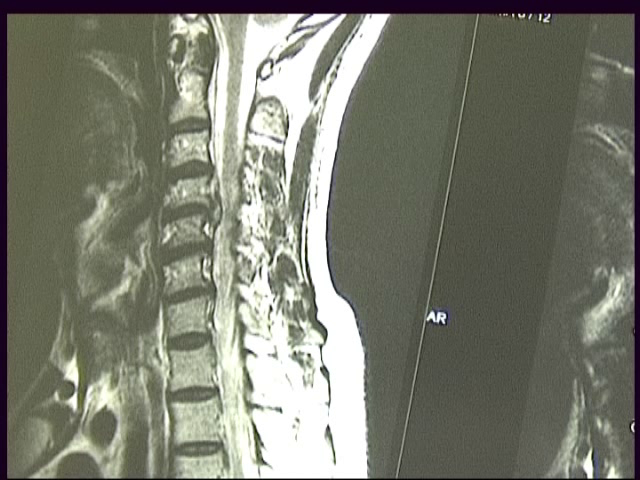
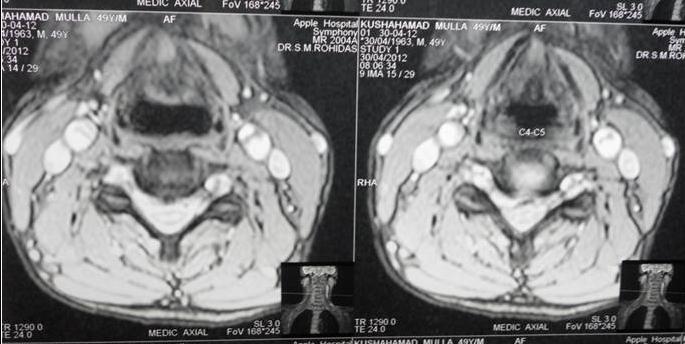
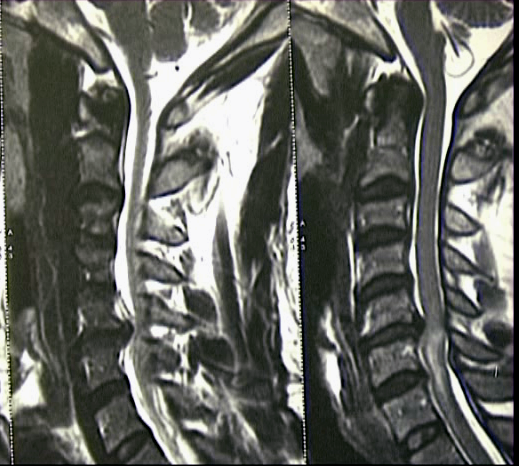
Pre-operative left C4/5 disc herniation Sagittal and axial view.

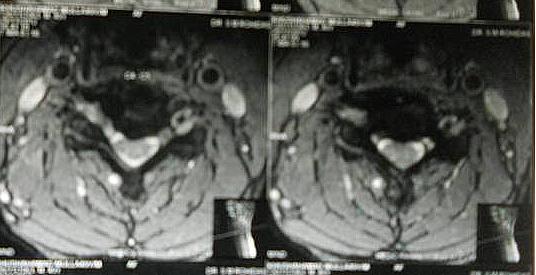
Post-operative Sagittal and axial view.
Endoscopic foraminotomy and vertebrectomy for cord decompression.
Compression of the cervical cord and roots in the elderly is often due to bony bars along the posterior and lateral surfaces of discs, thick osteophytes and thick, calcified posterior longitudinal ligament. Such patients usually show a heperintense signal in the spinal cord on T2 sequences of the MR scan due to myelomalacia. In such cases, once the exiting root is decompressed Endospine with endoscope is angulated medially to reach the anterior surface of cord. I use 2mm. drill bit for this and which keeps the drill tip under constant vision while working craniocaudal and axial mediolateral on the vertebral bodies. The posterior longitudinal ligament is exposed. Unless adequate craniocaudal decompression in transverse direction is achieved posterior longitudinal ligament is not opened. When there is a central disc herniation one can see tear in the posterior longitudinal ligament. Ossified posterior longitudinal ligament (OPLL) is removed with help of 2 mm Kerrison punch. I use the ultrasonic bone dissector/rasp to safely widen the bony window. Accidental slippage or kick back of the drill tip can be life threatening while working close to the cervical cord. For the safety of the important neural and vascular structures Ultrasonic bone dissector/rasp is used to remove bone. The window of bone is widened till the lateral edge of opposite dural sac is seen.
Closure
A small piece of gelfoam is kept in the foraminotomy. Outer tube is taken out. Platysma is sutured with 3 -0 vicryl and the skin with subcuticular sutures with 3 – 0 vicryl.

Skin Incision
Discussion
Conventional anterior cervical disc surgery has evolved over last 5 decades. Complete disc removal without bone graft, with bone graft for fusion and use of metal implant are some variations. The more recent usage of arthroplasty with artificial disc attempts to restore the mobile motion segment but requires discectomy.
Anterior endoscopic cervical surgery on discs and intervertebral foramina is a new technique using uncovertebral trajectory. It embodies the concept of functional spine surgery. (3). The aim of functional spine surgery is direct removal of the compressing lesions while preserving the motion segment of spine and the rest of the normal disc.
The antero-posterior inclination of cervical intervertebral discs as seen in the sagittal plane varies at different levels. I follow the disc from its anterolateral margin to the lateral edge of the dural sac. Also according to the cranial or caudal migration of the herniated disc I widen the bony window to expose the disc hernia.
Although the surgical risks of anterior cervical foraminotomy and cord decompression have been minimal in my experience, permanent and serious complications can occur as in any type of anterior cervical spine surgery. The major potential concerns include Horner’s syndrome, laryngeal nerve injury, vertebral artery injury, spinal instability and recurrent disc hernia.
The cervical sympathetic nerve and chain pass along the lateral margin of longus colli, Horner’s syndrome can occur if the sympathetic nerve is damaged while retracting these muscles or completely dividing them. Hence I remove a very small part of the medial edge of the longus colli muscle to expose the disc space. Horner’s syndrome can be temporary or permanent. Two of my patients developed Horner’s syndrome but both recovered completely in due course.
Injury to the vertebral artery is a risk in any anterior cervical approach. To avoid this injury one has to know the variations in the entry point of vertebral artery (commonly at C 6 ). The level of vertebral artery entry into the transverse foramen should be seen on preoperative MRI scan in order to avoid this injury. I use medial to lateral dissection for foraminotomy commencing the drilling from the medial edge. On entering the disc space one can go laterally rather than going from lateral to medial while drilling. This will keep a thin film of bone over the medial aspect of vertebral artery. For removal of this bone from the uncovertebral joint I use 2 mm. Kerrison punch with the cutting edge of the punch directed medially – away from vertebral artery. I use ultrasonic bone dissector to remove bone covering the vertebral artery. Ultrasonic bone dissector safely removes bone without any traumatic or thermal trauma to the artery. While removing bone medial to the vertebral artery with Kerrison punch there can be significant bleeding from the venous plexus around vertebral artery. It is not helpful to use endoscopic bipolar to stop oozing from the venous plexus. The best way is to put small piece of surgicel® medial to the vertebral artery in between the two adjacent transverse processes.
Another complication associated with this approach is leakage of cerebrospinal fluid. I have made a dural puncture during one of my operations. To prevent CSF leak I used fibrin glue over a small piece of muscle pushed carefully into the puncture.
Hoarseness of voice can be due to trauma to laryngeal nerve with retractor or trauma during the creation of the passage to the vertebral bodies. I have two patients with postoperative hoarseness of voice. One developed immediate after surgery. Intravenous methylprednisolone for three days was followed by complete recovery. The other patient had hoarseness of voice 2 weeks after surgery. It was seen when she came for follow up. Oral steriods for three weeks in tapering doses resulted in complete recovery of voice in 6 weeks.
Postoperative management
No cervical brace or collar is advised. Four hours after surgery, oral lozenges are prescribed to reduce throat pain and the patients are made to sit, stand and walk.Post-operative x-ray of the cervical spine is obtained to confirm stability and MRI performed to confirm adequate decompression. 80% patients were discharged the day after surgery.All patients are followed up every 15 days for two months, every two months for six month and then every 4 to 6 months for next one year.
Advantages of the surgical approach
- Direct access to the compressing lesion. Targeted surgery
- Preservation of the most of the disc tissue
- Does not require any sort of fusion
- Direct decompression of the nerve root and cord
- It can treat both soft and hard disc, root and/or cord compression
Advantages to the patient
- No need of cervical brace/collar after surgical procedure
- Shorter hospital stay
- Less postoperative pain in neck and arm
- Rapid return to normal activity
Advantages of Endospine system
- Mobility of the operating system as the endoscope, suction, and instruments move as a unit in constant relation to each other.
- HD television with zoom provides sharp panoramic vision.
- The surgeon obtains a focused, wide and enlarged view of the operative field.
Conclusions
Endoscopic anterior cervical nerve root decompression with foraminotomy and discectomy is a minimally invasive technique allowing one to remove herniating disc fragments and osteophytes with minimal damage. This method avoids osteoarthrodesis or arthroplasty with artificial disc. ( 7, 8, 9, 10 ). This technique is efficient with good results and low morbidity. The learning curve here is longer than with anterior or posterior approach but is rewarding given its advantage of preservation of the disc and motion segment.
References
Jho HD Microsurgical anterior cervical foraminotomy, a new approach to cervical disc herniation. J. Neurosurg. 1996; 84:155-160.
Jho HD, Kim WK, Kim MH. Anterior microforaminotomy for treatment of cervical radiculopathy: part 1- disc preserving “ functional cervical disc surgery.” Neurosurgery. 2002; 51(supplement 2); 46-53.
Jho HD. Decompression via microsurgical anterior foraminotomy for spondyloticcervical myelopathy. J. Neurosurgery. 1997; 86:121-126.
Jho HD. Spinal cord decompression via microsurgical anterior foraminotomy for spondylotic cervical myelopathy. Minimally invasive Neurosurgery. 1997;40(4): 124-129.
Jho HD. Ha HG. Anterior cervical microforaminotomy. Operative Tech Orthop 8;46-52,1998.
Michael Bruneau. Bernard George. Microsurgical cervical nerve root decompression by anterolateral approach. Operative neurosurgery 1 vol. 58, Feb 2006.
Edward CC 2nd, Heller JC, Murakami H : Corpectomy versus laminoplasty for multilevel cervical myelopathy. An independent matched cohort analysis, Spine 27: 1168-11752; 2002.
Emery SE, Fisher JR, Bohlman HH: Three level anterior cervical discectomy and fusion: Radiographic and clinical results, Spine 22: 2622-2625; 1997.
Lunsford LD, Bissonet DJ, Zorub DS: Anterior surgery for cervical disc disease Part 2: Treatment of cervical spodylotic myelopathy in 32 cases. J Neurosurgery 53: 12-19; 1980.
Wada E, Suzuki S, Matsuoka T, Miyamato S, Yonenobu K, Subtotal corpectomy versus laminoplasty for multilevel cervical spondylotic myelopathy: A long term follow up study over 10 yrs. Spine 26: 1443-1448; 2001.
Introduction
Last two decades have seen emergence of minimalism in spine surgery to minimize the approach related trauma of the tissue. MISS – “minimally invasive spine surgery” phrase is nowadays quite often used. In fact it is a misleading terminology, because MISS surgeries are potentially maximally invasive at the target area. There is no compromise in achieving the exact goal, that is adequate decompression of compressed neural structures in MISS. But the approach related trauma to surrounding tissue is minimized.
It really does not matter what technique you use to decompress the nerve root, if you fail to fully decompress the nerve root or introduce complications to the equation, you have failed to serve the patient.
- Ian MacNab
One should try to follow this principle in spine surgery. In minimally invasive spine surgery while following this philosophy each and every patient’s symptoms, clinical signs and radiology has to be evaluated separately and carefully. If the decompression of the compressed nerve root / cord is inadequate, then the compressive symptoms, signs will persist. If the decompression is aggressive or more than necessary then there are chances that the existing stability is compromised. Hence there has to be nice equilibrium between adequate decompression without compromising the existing stability. This equilibrium will be different for every patient, every level to be operated, extent of stability / instability & the pathology to be treated. This is dependent on each spine surgeon along with the technique used by the surgeon. This is one of the many factors which is responsible for steep learning curve in MISS – Endoscopic spine surgery.
Destandau’s technique
Dr. Jean Destandau M. D. neurosurgeon from Bordeaux France, developed a technique of endoscopic spine surgery in 1993. ( 1, 2). This technique is based on basic principle of laparoscopic technique of triangulation between an endoscope and suction with working instrument.
Basics of Endospine – Destandau’s technique
In Destandau’s technique we use Endospine, a set of outer tube / insert and inner tube / working insert with an endoscope. The endoscope used with endospine is 18 cm’s, long, rigid, straight, 0 degree endoscope. One can say an universal endoscope which used in cystoscopy, arthroscopy, sinoscopy etc. The outer tube is elliptical in shape rather than circular. Endospine was initially used for lumbar disc herniation. The target area in lumbar region is elliptical, in between two laminae, medially the spinous process and laterally the medial facet, hence the outer tube might be of elliptical shape rather than round. The inner tube / working insert fits in to the outer tube with a rachet type lock. There is an inherent telescoping movement in between these tubes.


The working insert has four in build channels inside. On the left side of the working insert it has two channels of 4 mm diameter which are parallel to each other. The medial 4 mm channel hosts the endoscope and then the endoscope remains fixed with lock. The second 4 mm channel is for suction tube. The largest channel of 9 mm is for working instrument. The channels for endoscope and suction, is at an angle of 12 degrees to the wide channel for instrument. Because of this angle we can use 0 degree endoscope as an angled scope. This helps in minimizing the fogging of endoscope tip. When the endoscope and the instrument are working parallel to each other there is intermingling of the instruments. And we have to use an angled endoscope when endoscope and instrument work parallel to each other. The fourth channel is for nerve root retractor to retract the nerve root medially so as to expose disc space. The outer tube and inner tube are fixed in such a way that there is an artificial space created in between the two tubes. This is the working space for the instruments. Once the excision of the bone is achieved then the inner tube can be pushed inside/down. If there is no space maintained in between the outer tube and inner tube then the endoscope will touch to the tissue in front and will hamper the vision. Also there will be splashing of fluid over the endoscope lens if adequate space is not maintained in between these tubes. The suction is used with left hand and working instrument is in the right hand. With suction in left hand surgeon can move whole system in medial, lateral, cranial and caudal direction. Same movements are possible with instrument in right hand. The suction in left hand and instrument in right hand work as breaks for the system to maintain the stability of the system. When the surgeon is using suction to clean the operative area, the instrument in right hand keeps the system stable, vice versa when surgeon is using instrument, suction in left hand keeps the system stable. This synchronisation of movements of both hands, is necessary while looking at the image on the screen. Surgeon should learn this synchronisation of both hands movements, along with using of both hands while looking at the screen image. This is the basic’s of the Destandau’s technique is spine surgery.
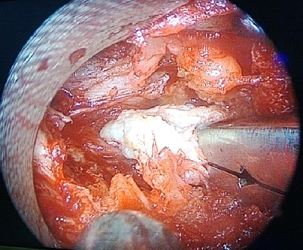
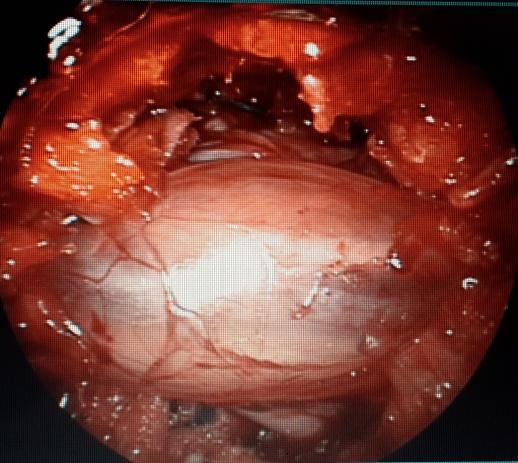
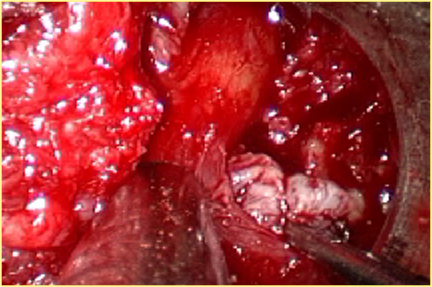
Endospine can be used for this indication once sufficient experience is gained. Small intradural extramedullary tumors mostly posterior or lateral can be excised. Anteriorly placed tumors in thoracic region are difficult. Exact localization of the level is done with localizing pin and C arm. Rather than paramedian incision midline incision is preferred. Subperiosteal dissection of muscles with excision of spinous process is done. Then outer tube with two small retractors is fixed with endospine system. Under endoscopic vision laminectomy performed with Kerrison punch. Over the lateral edge of dural sac small thin gelfoam is placed so as to control the epidural oozing, rather than cauterizing the epidural veins. Dura is opened with 15 mm knife and then incision is extended with scissor. Two stay sutures are taken on dural edges through outer tube. For this paediatric laproscopic needle holder with outer tube is used. 4-0 vicryl with round body needle is used. Again the outer tube is placed with stay sutures retracting the dural edges. If the localization is correct with no shift of the SOL due to positioning, then mostly SOL is seen compressing cord. Dissection of SOL is done with small curettes, endoscopic angulated cautery. Attachment of nerve root is resected with scissor or cautery. SOL is taken out carefully by holding it with biopsy forceps along with whole endospine system. In case of a firm tumour like meningioma ultrasonic tumour dissector can be used to suck out the exposed tumour with minimal surrounding tissue trauma.



Closure of dura is achieved with 2 mm titanium anaestoclips. These are used in cardiac surgery to closed arterial walls. The dural stay suture holds the dural edges together and shaft of anaestoclips is sufficiently slender which can be passed through working channel of endospine.
Muscle and skin are closed with 2 0 vicryl.